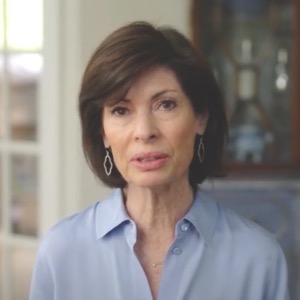
I would like to introduce my daughter Sabina Paradi.
She was a dietetic fellow at Columbia University, New York Hospital, in 2007 when she sustained traumatic brain injury after being struck by a truck in New York’s Lower West Side on the way from a play.
The system worked perfectly when she was assisted immediately by a passing nurse. In minutes she was dispatched via ambulance by a fine paramedical team and was brought for evaluation in the hospital.
This is where the system broke down. The immediate reaction by the team was to attempt to relieve acute elevated intracerebral pressure. The method chosen, hemicraniectomy, and the anesthetic (propofol) were both inappropriate to her care. Hemicraniectomy has been shown in a later study to be inappropriate in most cases. Propofol has been banned by the FDA in the treatment of pediatric traumatic brain injury patients because of various complications. My daughter was very slight of build, under 100 lbs, easily smaller than many pediatric cases. She was also athletic, which may have increased the tendency for higher intracerebral pressure. She had been ill for over a week, having contracted a resistant infection from one of her patients, and was taking antibiotics.
How would systems improvement have helped at this stage? Her condition should have been evaluated by a higher level of expertise, and used tools like teleconferencing and remote medicine to get the opinion of a nationwide team of experts. The hospital throughout her care lacked access to medical expertise other than what appeared to be a very overworked neurosurgeon. Traumatic brain injury cases in the first hours require extraordinary care in their evaluation.
What happened next? What happened next, I believe, is responsible for her death. She contracted a resistant pneumonia which was identified with her respirator. Complicating everything was that she was taking antibiotics, and therefore immunosuppressed; she had a head injury and was therefore immunosuppressed; she sustained extensive neurosurgery and was therefore immunosuppressed; and she was sedated and therefore immunosuppressed. The infections deepened her coma, along with the sedation.
Risking surgery and sedation in her case was very much contraindicated. There were and are many alternate protocols for handling cases like hers. Greater knowledge and the use of artificial intelligence might have led to an entirely different treatment regime. Other items needed were immediately accessible MRI, preferably state of the art; real-time polymerase chain reaction tests for the detection of microbial infections, in particular fungal infections which seem to plague the immunosuppressed; and a modern neurological intensive care facility. The facility at my daughter’s hospital had a ward shared among four neurologically impaired patients, all quite likely immunosuppressed.
In the end, what killed my daughter was a complete lack of knowledge of her condition which instrumentation and broader, specialized knowledge would have alleviated. Facilities like the US military traumatic brain injury facility at Ramstein, Germany, are more appropriate to the treatment of moderate to severe traumatic brain injury than hospital emergency rooms. It is my view that all such patients should be evacuated to very large specialty hospitals that treat only severe neurological conditions such as stroke, TBI, encephalitis, and the like. Air transport systems and stabilization protocols need to follow the military model.